Will protein help me lose weight? Should I include it in every recipe and eat it at every meal? Could too much damage my kidneys? At Precision Nutrition, our inbox is filled with questions about the pros and cons of eating more protein. In this article we’ll set the record straight, so you can finally separate the facts from the fiction.
++++
MAYBE YOU’RE A PROTEIN PROMOTER.
You buy protein powder in “bucket with a handle” format. You know the protein counts of every food you eat.
After every workout, you jam those amino acids into your cells. You swear you can feel them getting swole.
OR MAYBE YOU’RE A PROTEIN AVOIDER.
Maybe you’ve heard bad things.
Like: Protein will damage your kidneys.
Or: Protein will give you cancer.
Or simply: We all eat too much protein.
Maybe you want to experience a fitness transformation: lose fat. Or gain muscle. Or be healthy.
You just want to do the right thing and eat better. But with conflicting information about protein, you don’t know what to think.
Or, if you’re a fitness and nutrition coach, you’re wondering how the heck to clear up the confusion about protein among your clients.
Let’s get into it.
In this article, we’ll explore:
- What are high-protein diets?
- What does the evidence say about high-protein diets and health?
- Does protein source matter?
- How much protein is right for me?
How to read this article
If you’re just curious about high-protein diets:
- Feel free to skim and learn whatever you like.
If you want to change your body and/or health:
- You don’t need to know every detail. Just get the general idea.
- Check out our advice at the end.
If you’re an athlete interested in performance:
- Pay special attention to the section on athletic performance.
- Check out our advice for athletes at the end.
If you’re a fitness pro, or interested in geeking out with nutritional science:
- We’ve given you some “extra credit” material in sidebars throughout.
- Check out our advice for fitness pros at the end.
Why protein?
A quick intro if you aren’t a nutrition pro:
- Protein is one of the three main macronutrients that makes up the food we eat. (The other two are fat and carbohydrate.)
- Protein itself is made up of amino acids.
- Amino acids are the building blocks for most stuff in our bodies. They’re like Legos that can be broken down and re-assembled in different ways.
- Unlike extra fat (which we can store very easily on our bums and bellies), we don’t store lots of extra amino acids. Protein is always getting used, recycled, and sometimes excreted.
- If we don’t get enough protein, our body will start to plunder it from parts that we need, such as our muscles.
- So we have to constantly replenish protein by eating it.
We need protein.
Protein is so important that without it, we die or become seriously malnourished.
(This protein-deficiency disease is known as kwashiorkor, and we often see it in people who have suffered famines or who are living on a low-protein diet.)
All your enzymes and cell transporters; all your blood transporters; all your cells’ scaffolding and structures; 100 percent of your hair and fingernails; much of your muscle, bone, and internal organs; and many hormones are made of mostly protein. Hence, protein enables most of our bodies’ functions.
Put simply, you are basically a pile of protein.
No protein, no you.
How much protein do we need?
Short answer: It depends.
Let’s look first at the current Recommended Daily Allowance (RDA).
The RDA for protein is 0.8 g/kg (0.36 g/lb) — the more you weigh, the more protein you need:
- A 150-lb (68 kg) person would need 68 x 0.8, or about 54 grams of protein a day.
- A 200-lb (91 kg) person would need 91 x 0.8, or about 73 grams of protein a day.
That generally works out to about 10 percent of daily calories coming from protein.
However.
RDAs were originally developed as a way to prevent malnutrition — to represent the minimum amount of a nutrient we need to not die (or get sick).
“You’re not dead” is not the same thing as “You’re kicking ass.”
The RDA for surviving may be different than what we need to thrive.
The RDA is also a very general recommendation. It doesn’t take other things into account, such as:
- How much total energy (i.e. calories) we eat or need
- Our carbohydrate intake
- When we eat the protein
- Our biological sex
- Our age
- How active we are
- What activities we do
- How “eco-friendly” various protein sources are
The Institute of Medicine (US) suggests a huge range in individual protein requirements — from 0.375 g/kg to 1.625 g/kg body weight (0.17 to 0.74g/lb body weight).
In other words, our hypothetical 150-lb person might have protein needs ranging from 26 to 111 grams per day.
Well that narrows it down nicely, doesn’t it!?
Let’s take a deeper look: Amino acidsProtein in our food is made up of many different building blocks, or amino acids.
Most people focus on Recommended Daily Allowance (RDA) for total protein, but they don’t think about how much of each amino acid they might need.
If your diet isn’t varied enough, you may be eating enough total protein, but not enough of a specific essential amino acid.
Every day, you need this much of these essential amino acids:
- 14 mg/kg of histidine
- 19 mg/kg of isoleucine
- 42 mg/kg of leucine
- 38 mg/kg of lysine
- 19 mg/kg of methionine + cysteine
- 33 mg/kg of phenylalanine + tyrosine
- 20 mg/kg of threonine
- 5 mg/kg of tryptophan
- 24 mg/kg of valine
Of course, you don’t need to spend hours in your kitchen with an eyedropper of lysine solution, carefully calibrating your intake.
Just eat a variety of protein-rich foods and let nature do the rest.
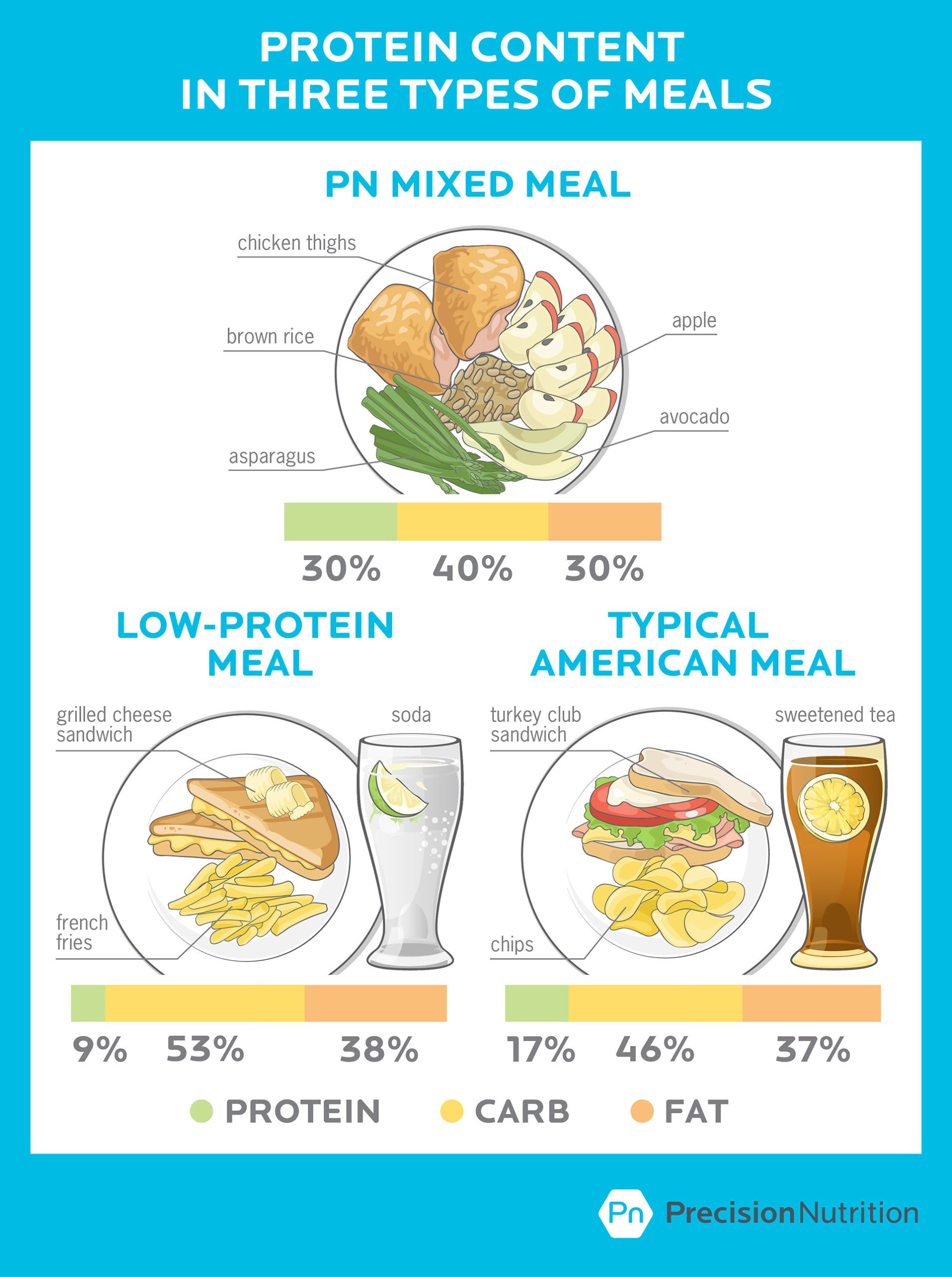
What does a high-protein diet look like?
People often assume that “high protein” means “low carbohydrate”. In fact, you can eat more protein without making any drastic changes to other things in your diet.
Many types of diets can be considered high-protein. “High protein” is a bit of a relative concept; there’s no clear rule.
The average protein intake for adults in the US is about 15 percent of calories coming from protein.
The Institute of Medicine suggests that up to 35 percent of total calories is an OK proportion of protein for healthy adults.
And most researchers would say that once you get more than 25 percent of total calories from protein, you’re in “high protein” territory.
Here’s what high- and low-protein diets might look like for a given meal.
The upper tolerable limit (UL) of something tells you how much you can eat without having health problems.
Currently, there’s no established UL for protein.
Does that mean you can eat as much protein as you’d like without any negative side effects? No. It just means researchers haven’t figured it out yet.
But we do know that eating up to 4.4 g/kg (2 g/lb) body weight didn’t cause any short term health problems in clinical studies.
Let’s take a deeper look: Calculating maximum proteinThe Institute of Medicine suggests that high protein intake, where about 35 percent of your calories comes from protein, is safe.
What does that mean in grams per kilogram body weight (or g/lb body weight)?
Say you’re 74.8 kg (165 lb) and reasonably active. You need about 2,475 calories per day to maintain your weight.
If you get 35 percent of your total energy intake from protein, you’d be eating about 866 calories from protein each day.
1 gram of protein has 4 calories. So 866 calories is around 217 grams of protein per day.
That’s about 1.3 grams per pound of body weight, or 2.9 g/kg.
Will eating a high-protein diet hurt me?
For years, people have been concerned with the safety of eating too much protein.
Will eating too much protein explode my kidneys?
How about my liver? My left femur?
The most common health concerns of eating more protein are:
- kidney damage
- liver damage
- osteoporosis
- heart disease
- cancer
Let’s explore these.
Claim: High protein causes kidney damage.
This concern about high protein and kidneys began with a misunderstanding of why doctors tell people with poorly functioning kidneys (usually from pre-existing kidney disease) to a eat a low-protein diet.
But there’s a big difference between avoiding protein because your kidneys are already damaged and protein actively damaging healthy kidneys.
It’s the difference between jogging with a broken leg and jogging with a perfectly healthy leg.
Jogging with a broken leg is a bad idea. Doctors would probably tell you not to jog if your leg is broken. But does jogging cause legs to break? No.
That’s the same thing with protein and kidneys.
Eating more protein does increase how much your kidneys have to work (glomerular filtration rate and creatinine clearance), just like jogging increases how much your legs have to work.
But protein hasn’t been shown to cause kidney damage — again, just like jogging isn’t going to suddenly snap your leg like a twig.
High-protein diets do result in increased metabolic waste being excreted in the urine, though, so it’s particularly important to drink plenty of water to avoid dehydration.
Verdict: There’s no evidence that high protein diets (2.2g/kg body weight) cause kidney damage in healthy adults.
Claim: High protein causes liver damage.
The liver, like the kidneys, is a major processing organ. Thus, it’s the same deal as with kidneys: People with liver damage (such as cirrhosis) are told to eat less protein.
Yes, if you have liver damage or disease you should eat less protein. But if your liver is healthy, then a high-protein diet will not cause liver damage.
Verdict: There’s no evidence that high-protein diets (2.2g/kg body weight) cause liver damage in healthy adults.
Claim: High protein causes osteoporosis.
Eating more protein without also upping your fruit and vegetable intake will increase the amount of calcium you’ll lose in your pee.
That finding made some people think that eating more protein will cause osteoporosis because you’re losing bone calcium.
But there is no evidence that high protein causes osteoporosis.
If anything, not eating enough protein has been shown to cause bone loss. Bones aren’t just inert sticks of minerals — a significant proportion of bone is also protein, mostly collagen-type proteins.
Like muscle, bone is an active tissue that is constantly being broken down and rebuilt. And like muscle, bone needs those Lego building blocks.
Women aged 55 to 92 who eat more protein have higher bone density. So eating more protein improves bone density in people most at risk of having osteoporosis.
(Eating more protein plus adding resistance training: Double win for bone density.)
Verdict: High protein diets do not cause osteoporosis, and actually may prevent osteoporosis.
Claim: High protein causes cancer
Unfortunately, we still don’t have conclusive human studies on the cause of cancer and the role of protein.
There are studies that asked people how much protein they ate over their lifetime, and then looked at how often people got cancer. The research shows a connection between protein intake and cancer rates.
But these studies are correlational studies and don’t prove that protein is the cause of cancers. Plus, some researchers have gone so far to say that studies relying on subjects to recall what they ate are basically worthless because human memory is so inaccurate.
A big part of the proposed cancer and protein link comes down to confounding factors, like:
- where you get your protein from — plant or animal
- how you cook your protein (i.e. carbonized grilled meat)
- what types of protein you’re eating (e.g. grass-fed steak versus a hot dog)
And so on.
In other words, we can’t say that any particular amount of protein causes cancer.
Verdict: Limited evidence that protein causes cancer; many other confounding factors.
Let’s take a deeper look: Protein and cancerA study from 2014 looked at protein and cancer risk. It was widely misinterpreted as proof that eating a lot of protein caused cancer.
First, it was actually two studies, one asking people questions and following them for years; and one that fed mice a high-protein diet and implanted them with cancer.
With the human study, researchers looked at people’s self-reported protein intake and their rates of cancer over the following 18 years.
They found that people aged 50-65 who ate diets high in animal protein (≥20% of total calories) had a 4-fold greater risk of dying of cancer over the next 18 years compared to people who ate a moderate amount of protein (10-20% of total calories).
(Just so you get an idea, smoking increases your risk of cancer by 20-fold.)
Then, it gets more interesting, because for people over 65, eating more protein decreased cancer risk by more than half. In summary:
Eating more protein from 50-65 years old was associated with a higher risk of death from cancer, but over 65 years old that association was reversed.
The second part of the study is where people really misunderstood what the study had proven.
Researchers fed mice a high-protein diet (18% of total calories), then implanted cancerous cells. They found that the high-protein diet increased tumor size. This is not a surprise, since protein increases IGF-1 (an anabolic protein) that stimulates growth in pretty much all tissues, including cancerous tissue.
Higher protein diets stimulated cancerous growth in mice.
So, while eating more protein might increase the size of existing tumors (depending on what treatment someone is undergoing), this study does not show that high-protein diets cause cancer.
Claim: High protein causes heart disease.
Eating animal-based protein daily is associated with an increased risk of fatal coronary heart disease (70 percent for men and 37 percent for women), whereas plant-based proteins aren’t linked to higher rates of heart disease.
This suggests that where you get your protein from may matter more than how much protein you eat.
However, just like cancer, the link between heart disease and high-protein diets is from questionnaires rather than a double-blind randomized study (the gold standard in research).
There are many confounding factors. For one, consider the type of animal — does seafood cause the same issues as red meat, for example?
We don’t yet know the whole story here.
Verdict: Limited evidence that protein causes heart disease and the source of protein is a major confounding factor.
Let’s take a deeper look: Protein sourceA new study in the Journal of American Medical Association (JAMA) looks not only at protein intake, but where people got their protein from.
More than 131,000 people were asked:
- how much protein they ate; and
- if it came from animals or plants.
This study took over 35 years to do (starting in the 1980s).
What they found:
Eating more animal protein was associated with a higher risk of death… if you were also doing something else that was a risk factor.
Such as:
- smoking
- being overweight
- not exercising
- drinking alcohol
- history of high blood pressure
- low intake of whole grains, fiber, and fruits and vegetables
Eating more plant protein was found to be associated with lower risk of early death.
What does this mean?
You might think at first glance that you should eat less animal protein, since this study seems to say that animal protein is bad for you.
But there’s more to it.
If you’re doing everything else “right”, then eating more animal protein doesn’t seem to be a problem.
Likely, it’s not the animal protein on its own but a lot of lifestyle things that come with eating more animal protein.
For instance, this study began in the 80s. At that time, nearly every doctor told their patients to eat less fat and meat, and to avoid eggs.
So if you were a somewhat health-conscious person, then you’d likely be eating less animal protein compared to someone who was less health-conscious (or if you went against your doctor’s advice) — but you’d also likely be engaging in a bunch of other health-supporting decisions and activities.
The problem with these types of studies, called correlational studies, is that you can never be sure whether the associations are caused by one onto the other or if they’re simply happening at the same time.
Protein quality matters
Most people think about how much protein, but they don’t think all that much about the quality of the protein they’re eating.
There are huge differences in the chemical makeup of a given protein source, and how valuable that protein is nutritionally.
The higher a protein’s quality, the more easily it can give your body the amino acids it needs to grow, repair and maintain your body.
The two big factors that make a protein high or low quality are:
- Digestibility:
- How easy is it to digest?
- How much do you digest — and absorb and use?
- Amino acid composition:
- What amino acids is it made of?
A high-quality protein has a good ratio of essential amino acids, and allows our body to use them effectively.
Amino acid composition is more important than digestibility.
You can have way more protein than you need, but if the protein you’re eating is low in an important amino acid (known as the limiting amino acid), it causes a bottleneck that stops everything else from working (or at least slows things down).
High-quality proteins have more limiting amino acids, which means the bottleneck is lessened and our bodies can use that protein source better.
Let’s take a deeper look: Measuring protein’s worthScientists use many ways to calculate protein quality, or how well we might digest, absorb, and use a given protein.
Here are a couple.
Protein Digestibility Corrected Amino Acid Score (PDCAAS)
PDCAAS is calculated using a ratio of limiting amino acids and a factor of true digestibility to give you a value that lets you know how much of a given protein is digestible.
The higher the score, the higher the quality of protein.
PDCAAS is the current gold standard for measuring protein quality, but there are a few other protein quality scoring methods that we cover in the Precision Nutrition Level 1 Certification program.
Indicator amino acid oxidation (IAAO)
When we don’t have enough of a particular indispensable amino acid, then all the other amino acids, including that indispensable one, will be oxidized (i.e. essentially wasted) rather than used for stuff like repairing tissues.
It’s kind of like a team sport: You can’t play without the goalie, so all the players sit around twiddling their thumbs, even though they’re all great players in their own right.
But if we’re getting enough of that particular amino acid, then we won’t see all that oxidation. We have a goalie and the rest of the players can play.
So, you want the IAAO score to be low, indicating that all your amino acids are doing their jobs to rebuild you.
Thus far, the IAAO method seems like a very useful way to judge the metabolic availability of amino acids from different protein-containing foods, and to determine total protein requirements for all kinds of people.
New assessment techniques like IAAO are giving us a more precise idea of protein use, which means that we may see recommendations change in future.
Most likely, based on these recent findings, the RDA for protein will increase — i.e. doctors may tell us to eat more protein.
“Complete” and “incomplete” proteins
Back in the day, scientists used to talk about “complete” and “incomplete” proteins.
If you had a plant-based diet (i.e. vegetarian or vegan), you were told that you had to eat a mix of incomplete proteins (i.e. protein from a variety of plants) at each meal in order to meet your needs.
We now know this isn’t true.
As long as you eat a mix of different protein sources, you’ll get all the amino acids you need. No need for mealtime protein algebra to make sure you’re getting all your amino acids.
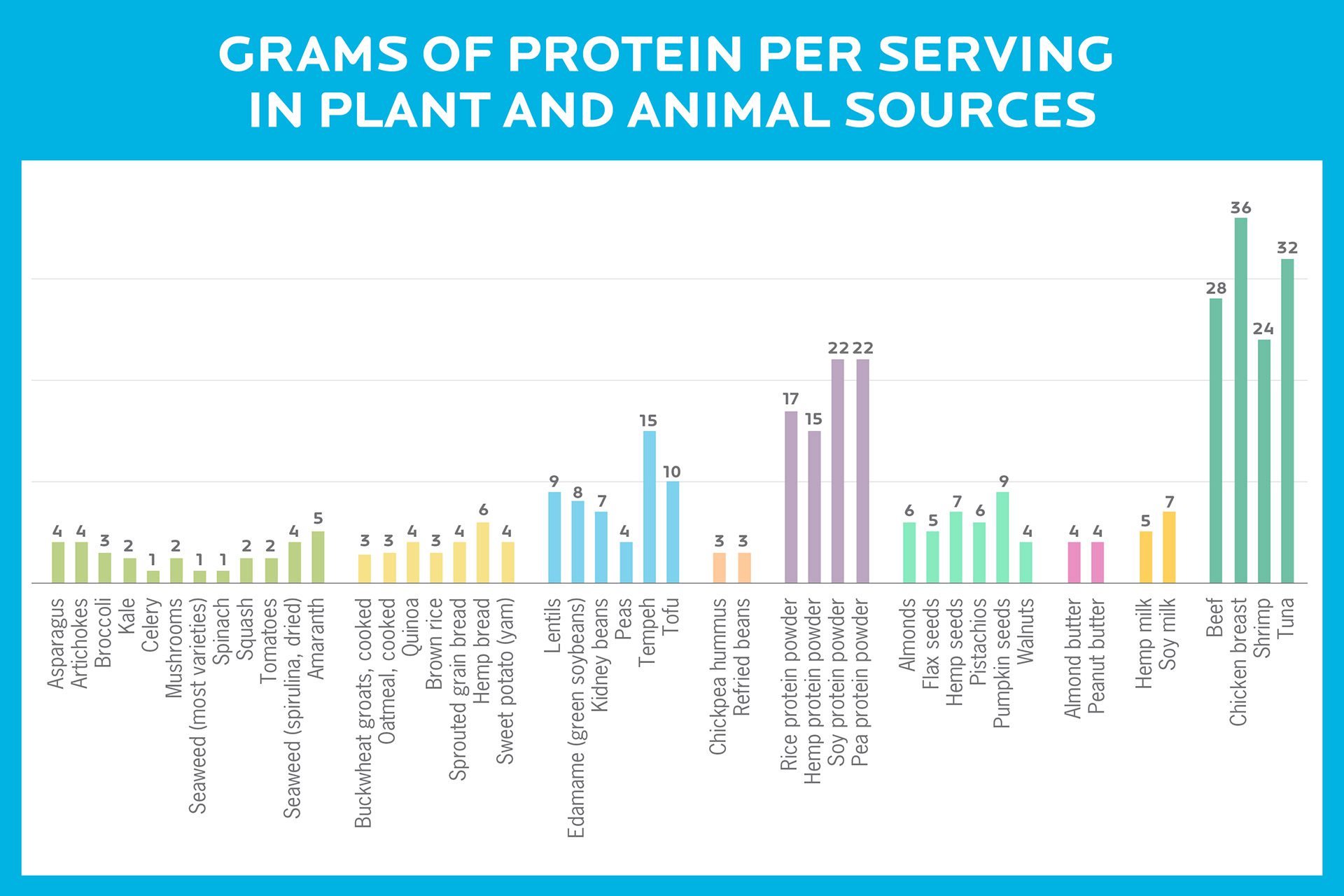
That being said, many plant-based sources are less protein-dense than animal sources. So if you choose not to eat animal products, you’ll have to work a little harder to get more protein from a wide variety of plant sources to make up the difference and meet your protein needs.
Animal vs. plant proteins
More and more, it seems that where you get your protein has a huge impact on your health.
Eating a high-protein plant-based diet improves health outcomes compared to low-protein diets and high-protein animal-based diets. Again, it comes down to the quality of your protein more than how much protein you’re eating.
If you’re a diehard carnivore, no worries — just add some more plant protein to your diet. Diversity is good. Hug some lentils today.
Why might you eat MORE protein?
Since we need protein to grow, maintain, and repair our tissues, hormones and immune system, there are times we need more protein.
The standard RDA of 0.8 g/kg is great if you’re sedentary and not building or repairing your tissue.
But you may need more protein if you are:
- physically active, either through workouts or your job
- injured or sick
- not absorbing protein normally
- pregnant / breastfeeding
- younger (and growing)
- older (and potentially losing lean mass)
Higher protein diets can also:
- lower blood pressure;
- improve glucose regulation;
- improve blood cholesterol; and
- improve other indicators of cardiometabolic health.
Win all around.
Here are some specific scenarios that might call for more protein.
Protein for athletes
Athletes and active people should eat more protein, but we don’t know exactly how much more.
The current recommendations vary from 1.2 to 2.2 g/ kg of body weight.
The International Society of Sports Nutrition says a range of 1.4-2.0 g/kg is safe and may help with recovering from exercise.
It looks like 2.2 g/kg (1g/lb of body weight) is the highest recommendation, but this shouldn’t be confused with the idea that more than 2.2 g/kg is unsafe.
More may not be necessary, but there is little evidence that more is unsafe.
Protein for aging
As you get older, you lose lean mass — both muscle and bone. This affects how long you live, as well as how functional and healthy that life is.
New research shows that most older people, particularly women over 65, need more protein than the current recommendations to slow down muscle loss.
Experts now recommend over 2.0 g/kg of body weight for people older than 65.
Protein for building muscle
The more protein in your muscles, the bigger and stronger your muscles can get.
Bodybuilders have long known that there is an “anabolic window” after a workout (24-48 hours) during which muscles are especially greedy for amino acids.
So, if you’d like to build muscle, make sure you eat a protein-rich meal within a few hours after training. Some advanced folks also like to add branched-chain amino acids (BCAAs) or essential amino acids (EAAs) as a during-workout or after-workout supplement.
Here, it seems that a fast-digesting animal protein supplement (whey) is better at getting your body to make more muscle compared to plant-based protein (soy). Of course, you can also just eat “real food” after working out.
Protein for losing fat
Eating protein helps with losing fat, for a few reasons.
1. When you eat more protein, you tend to feel fuller longer.
Protein stimulates the release of satiety (stop-eating) hormones in the gut. So when you eat protein, you naturally tend to eat less, without feeling hungry.
(You can test this theory if you want. Go and try to eat an entire plain skinless chicken, or a few pounds of lean fish.)
2. Protein makes your body work to digest it.
Not all nutrients take the same energy to digest. Fat and carbohydrates are pretty easy for your body to digest and absorb, but protein takes more energy to digest and absorb.
If you eat 100 calories of protein, you’ll only use about 70 calories of it. (This thermic, or heat-producing, effect of protein is why you sometimes get the “meat sweats” after a big protein-heavy meal.)
3. Protein also helps you hang on to lean mass while you’re losing fat.
When you’re in a significant energy deficit (i.e. eating less than you burn), your body tries to throw out everything — fat, muscle, bone, hormones, etc. — all the stuff you need. It doesn’t tend to throw out just fat and keep muscle… unless you eat lots of protein.
Let’s take a deeper look: Protein, lean mass, and energy restrictionA recent study at McMaster University in Canada explored what would happen if people who were on a very low-calorie diet (about 40 percent less than normal energy needs), ate a lot of protein, and worked out hard.
For 4 weeks, a group of young men in their 20s were basically starved, but on a high-protein diet — about 2.4 g/kg.
So, for instance, a 200 lb (91 kg), relatively active young man whose energy needs would normally be 3000 calories per day might get:
- 1800 calories per day (40 percent less than normal)
- 218 grams of protein per day (2.4 x 91 kg)
This means that out of those 1800 calories per day, about 48 percent of them were from protein.
The men trained hard — lifting weights and doing high-intensity intervals 6 days a week.
After 4 weeks, on average:
- The men gained about 1.2 kg (2.6 lb) of lean body mass (LBM).
- They lost about 4.8 kg (10.5 lb) of fat.
The fact that they lost fat isn’t surprising, though that amount of fat loss in 4 weeks is pretty impressive.
What is surprising is that they gained LBM.
There was a control group, who ate more of a normal-protein, low-energy diet — about 1.2 grams of protein per kg (so, for our 200 lb / 91 kg man, that would be around 109 grams per day). This group, on average:
- Gained 0.1 kg (0.2 lb) of LBM
- Lost 3.5 kg (7.7 lb) of fat
This study was only 4 weeks long, and on a specific population group under close supervision, but it’s a cool experiment that suggests protein might be able to do some nifty things even under difficult and demanding conditions.
It’s particularly useful because it’s a randomized controlled trial. In other words, it’s not a food questionnaire where you try to remember what you ate last year — it’s a direct comparison of two similar groups whose food parameters are being closely monitored.
We don’t recommend a highly restrictive, high-protein diet combined with a Spartan-style workout plan as a long-term strategy, but if you want to try something crazy for 4 weeks, see if you can replicate these results!
Why might you eat LESS protein?
Protein and longevity
Everybody is looking for the elixir of life; from 17th-century chemists to Monty Python.
And for years, living in a semi-starvation state has been shown to increase lifespan in nearly every animal from flatworms to rats to humans.
Looking into it more closely, it looks like restricting protein rather than calories, is the key to longevity.
Protein is anabolic: It triggers your body to build more tissues and other body bits. This is great if you want to build muscle, but there’s seems to be a downside: Eating protein triggers the body to release and make more IGF-1. In some people, this decreases longevity.
There’s a lot of work on lower IGF-1 and longer lifespan in animals (flatworms, rats and mice mostly) and some in people.
But it’s more complicated than saying that less protein leads to less IGF-1, which means living longer. There’s a genetic component. Some people do better with more IGF-1. In their case, more IGF-1 later in life actually increase lifespan.
And in terms of quality of life and functional longevity, a higher protein intake is probably still better. A semi-starved body may indeed live longer… but probably not better.
Age-related muscle loss alone could have serious consequences for metabolic health and mobility.
So: It’s difficult to say whether this is a good idea, despite interesting data. We probably need more research to say for sure.
What this means for you
If you’re a “regular person” who just wants to be healthy and fit:
- Follow Precision Nutrition’s portion recommendations.
We suggest a portion of lean protein at every meal, to keep that protein pool full and ready to help your body repair and rebuild.
- Try different kinds of protein.
Expand your repertoire and menu. This will help you get the best range of nutrients from real food.
- If you’re over 65, eat more protein.
This helps slow down age-related muscle loss, which improves long-term health and quality of life.
- If you’re a plant-based eater: Plan your meals carefully.
Without animal products, you’ll probably have to work a little harder to get enough protein. You might consider adding a plant-based protein powder to help yourself out.

You must be logged in to post a comment.